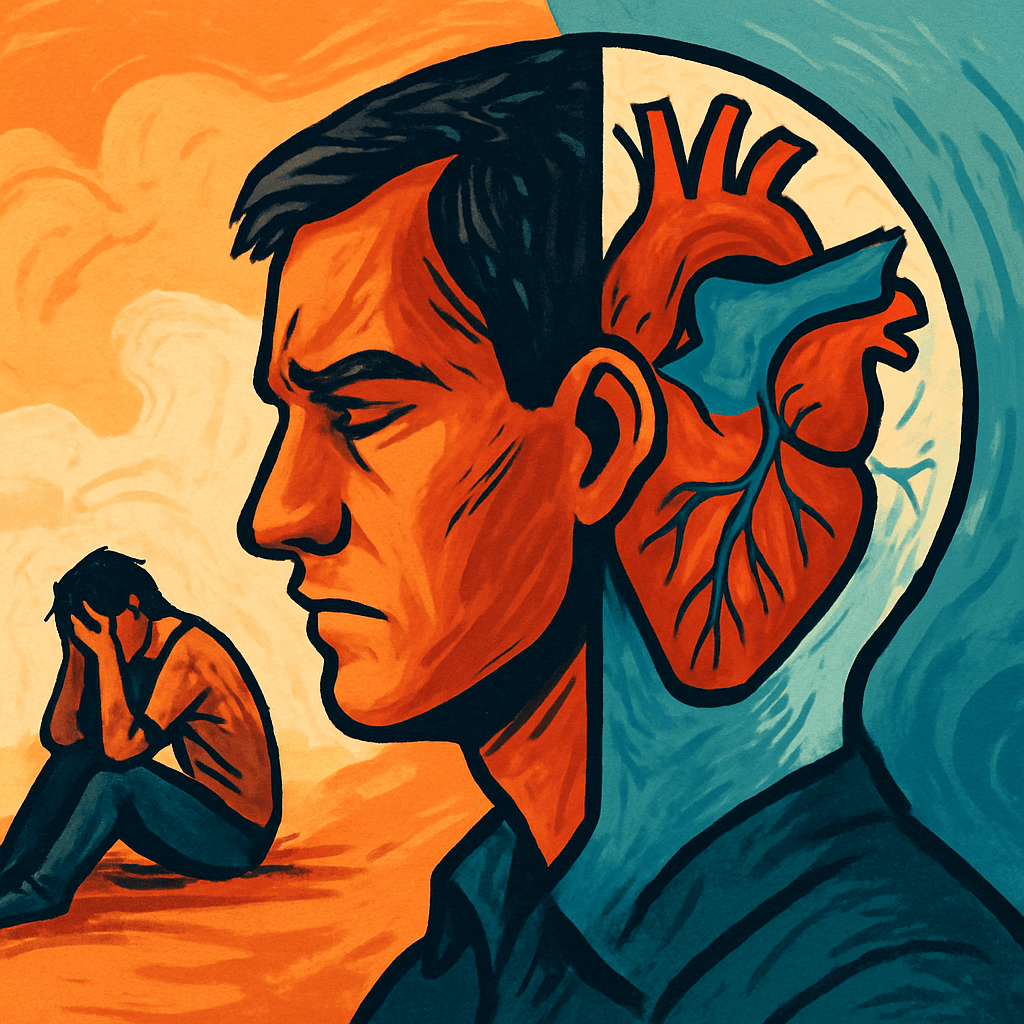
Heart disease risks spike with bipolar, anxiety, PTSD, and schizophrenia
– People with manic-depression bipolar disorder, anxiety, schizophrenia, and PTSD live 10-20 years less than those without.
The new study shows how these conditions double heart issues.
About one in four people faces a mental health issue in their lifetime; yet many go untreated, facing worse heart outcomes even though they have more doctor visits.
The new research, published in The Lancet Public Health in 2023, is an analysis of over 12 million patients across 24 countries.
Manic-depression bipolar disorder boosts heart disease odds by 57%, anxiety links by 41%, PTSD raises coronary risks by 61%, and schizophrenia hikes it 95%.
The disorders and heart problems reinforce each other. Chronic stress triggers body changes like inflammation, high blood pressure, and insulin regulation.
Behaviors frequently associated with mental health conditions worsen the risk. Higher smoking, less exercise, and unhealthy diets are more common among those affected.
Heart events, in turn, spark more mental issues. Depression strikes 18% of heart patients overall, surging to 28% after attacks. Nearly one in four stroke survivors battles depression, and 12% of heart attack victims develop PTSD.
Healthcare often fails those with mental health problems, because care is split between mental and physical care. This means cardiologists overlook mood symptoms, and psychiatrists skip heart checks. Patients get fewer screenings, meds, and procedures.
In the U.S., 2023 data shows 54% of those needing mental help got none, dropping below 45% for non-White groups. Even with universal coverage elsewhere, barriers like poverty and isolation block quality treatment.
Some things improve outcomes. Exercise, psychotherapy, and medicines reduce depression while bolstering heart health directly. Mind-body methods like yoga and meditation help symptoms and risks, though they lack proof against major events.
Experts say more should be done: train doctors on links between mind and body; expand insurance for screenings and treatments; and include mental health patients in heart trials for better guidelines. Without changes, disparities persist, robbing years from lives.
The connection between cardiovascular and psychological health calls for changes in the health care system to help improve outcomes for patients with co-morbidities, the lead author said.
For bipolar patients and families, vigilance matters. Mood swings can hide heart signs, so push for regular checks. Support healthy steps together, like walks and balanced meals, to fight both fronts.
The review sifts recent data from 2012 to 2024, drawing on meta-analyses and registries. It flags gaps: studies often exclude these patients or adjust unevenly for factors. More work needs tailored screens and therapies.
This story draws from a review in The Lancet Regional Health – Europe, published Sept. 2025.

Leave a comment