Device could improve treatment and drug safety for patients who take lithium for mania and depression
—Although lithium is first‑line medicine for acute mania and maintenance in bipolar I/II, the chemical has a narrow therapeutic window—too high a dose can be toxic to patients, causing kidney damage, thyroid damage, or even death, while too low a dose renders the treatment ineffective.
The dose of lithium varies between individuals based on body weight, diet, and other physiological factors, and requires regular measurement of lithium levels in the blood.
Currently, this is only available through standard laboratory-based blood draws, which can be time-consuming, inconvenient, and painful.
“Our goal was to create an easy-to-use sensor that bypasses the need for blood draws entirely,” says Yasser Khan, a USC professor. Khan leads the USC Khan Lab.
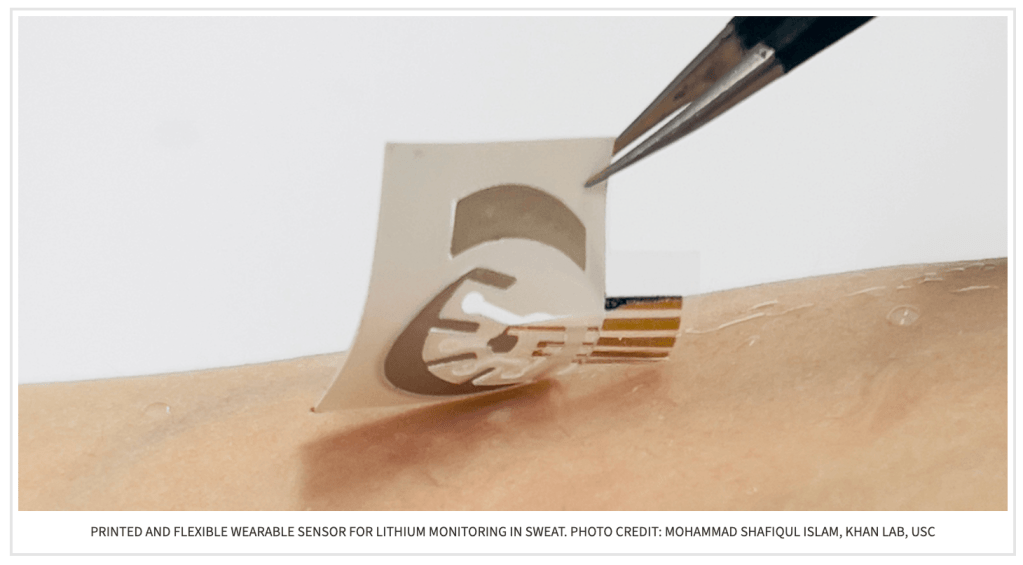
In the paper, “Wearable organic-electrochemical-transistor-based lithium sensor for precision mental health,” Khan’s team first identified sweat as an ideal alternative to blood samples as this fluid can be collected non-invasively and reflects lithium concentrations in real time.
The device induces sweat without requiring physical exertion. It collects data, which is transmitted to a smartphone app, allowing patients to conveniently track their lithium levels.
Behind this innovation: the use of organic electrochemical transistors (OECTs) specifically designed for lithium detection. OECTs are electronic devices that respond to ionic signals in liquid, converting them into readable electronic data.
The sensor’s potential extends far beyond the lab. In partnership with psychiatrist Adam Frank, MD, PhD, at the Keck School of Medicine, the device has already been tested by his patients.
“This is one of the biggest benefits of being at USC,” said Khan.
“We have clinical collaborators right across campus.” During pilot trials, Khan’s team worked directly with Frank and his patients to test the sensors in individuals taking lithium.
Sweat samples were collected using the wearable device, and lithium measurements were successfully matched against values derived from bulky commercial sensors. Participating patients responded positively, expressing relief at the prospect of monitoring their health without repeated hospital visits.
“The ability to non-invasively monitor lithium levels will improve care for patients taking lithium, who typically require regular blood draws to assess lithium levels. Being able to track these levels continuously over time will improve safety by allowing for medication dose adjustments that avoid side effects and potential medication toxicity,” said Frank.
Next, the team plans to develop more advanced wearable systems powered by artificial intelligence to automatically adjust lithium dosage and achieve optimal therapeutic benefits without causing lithium toxicity.
The research is published July 22, 2025 in the journal Device, a publication from Cell Press highlighting innovations in electrical engineering, materials science, and bioengineering.
Comment from a reader with bipolar disorder: While I have not tried taking lithium, I have met people who have been prescribed it for mania and experienced success with it. The number of regular blood tests required and possible liver damage make lithium worrisome to me. It’s good to see technological innovations, like this wearable device, that will help people maintain the correct blood levels of their medication to control the symptoms of mania in bipolar I.
Recent posts
- From Stranger Things to Real-Life Resilience: He confronts Bipolar Challenges
- Mental Health Experts Raise Alarms About AI Chatbots Fueling Psychosis
- AI Listens For Mood Swings In The Voices Of Those With Bipolar Disorder
- Hospital Visits For Hallucinogens Linked to Sharp Rise in Mania
- Jason Silva Says Hypomania is A Driver of Creativity

Leave a comment